Veterans, let us serve you!
It is important to understand that you MUST get the VA’s approval prior to seeking treatment at Sunrise. Even if we provide an assessment and determine that you meet criteria and you want to come to Sunrise, you still MUST get the VA’s approval before we can move forward. This is your responsibility. Here is how this should be done:
- Make an appointment with your VA Mental Health or Primary Care provider
- Ask for a referral to Community Care for Sunrise Rehab and Recovery at 1106 North Interstate 35, San Marcos, TX 78666
- Sunrise will facilitate things from there and coordinate with the VA as necessary
At Sunrise Rehab and Recovery, we want our admissions process to go as smoothly as possible for our Veterans. To keep the process simple, we take it step by step—emphasizing communication and transparency along the way. Throughout the entire process, we are ready to answer any questions about our drug and alcohol rehab center while offering our full support. The following outline highlights the four major steps in this process.
Start Your Recovery at Our Veterans Treatment Center
Sunrise Rehab and Recovery is ready to get you the help you not only need but deserve. Once admitted to our drug and alcohol rehab center, we will address the underlying issues of your condition while teaching you healthy coping mechanisms. This way, you can get sober and stay sober. It’s time to get on the path to recovery, so you can get back to having a healthy, fulfilling life. To learn more or to begin our admissions process today, please give us a call or use the contact form below.

TriWest Insurance Rehab for Veterans
Sunrise Rehab and Recovery is proud to accept TriWest Healthcare Alliance Insurance for Veterans. Past and present Members of the Military experience traumatic, life-threatening situations day-in and day-out. Because of the events Veterans and active members go through, it is important that as a Country, we cater to the ones who are protecting our Freedoms. Our Highly Credentialed Facility offers a welcoming and safe environment where individuals receive personalized treatment for their Drug & Alcohol Addiction and Co-occurring Disorders. Sunrise Rehab and Recovery is located in Beautiful, San Marcos, Texas.
ADMISSIONS AND ASSESSMENT PROCESS FOR VETERANS
Sunrise Rehab and Recovery / Sunrise Rehabilitation and Recovery is a Highly Accredited Addiction Treatment Center and TriWest Healthcare Provider. We treat Veterans and First Responders Struggling with Drug and Alcohol Addiction, PTSD, and Co-occurring Disorders.
Veterans
TriWest insurance, also called TriWest Healthcare Alliance, is a healthcare company that provides services for Veterans and military communities.If you are a Veteran suffering from the challenges of a substance Use Disorder, you may be able to access TriWest for assistance.
Community Care Network
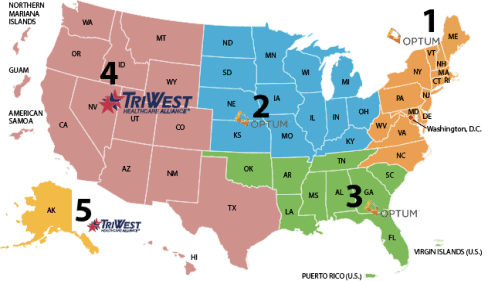
The VA Community Care Network (CCN) is VA’s direct link with community providers to ensure Veterans receive timely, high-quality care. CCN is comprised of five regional networks covering all U.S. states and. Once fully implemented, CCN will be the preferred national network VA uses to purchase care for Veterans in their community.
What is TriWest?
TriWest is a type of health insurance designed to help Veterans access healthcare in the United State. Established in 1966, the TriWest Healthcare Alliance helps administer services from the Department of Defense program, TRICARE.
In addition, TriWest VA insurance is administered through the Department of Veterans Affairs Community Care Network (VACNN) in certain regions.1 The Community Care network is a VA program to connect Veterans with private facilities when the VA facilities cannot meet their healthcare needs. The Community Care program helps:
Streamline all the VA’s community care programs into one program
Ensure Veterans receive good care in a timely manner
Develop relationships with community providers
The VACCN is operational throughout the United States and is separated into 6 different regions across the country.5 It’s important to determine which region you are in in order to take full advantage of the program. As part of the addiction services, Veterans can receive behavioral health care.
TriWest Eligibility Requirements
TriWest functions as a third-party administrator for Community Care partners in regions 4 and 5.3 This allows them to administer healthcare benefits for the VA system in the western United States, Texas, California, Alaska and more.
It’s important to understand that you must get the VA’s approval prior to seeking treatment, even though you may be eligible for TriWest insurance. The treatment is disbursed through the Community Care network, so it’s vital to be within their network. Here are the eligibility requirements for VA TriWest insurance:
You must have Community Care, which involves either being enrolled in VA benefits or be eligible for VA care without having to enroll.
Eligibility for Community Care is based on your individual health care needs or circumstances.
VA staff will determine who is eligible.
If you meet one of the following criteria, you may be eligible:
You’re a veteran needing services not offered at a VA center.
You live in an area that doesn’t have a full-time VA facility.
You are eligible to be grandfathered in.
The VA cannot deliver appropriate care in your case.
It’s in your best interest to be connected with a facility.
A VA service line is not fulfilling quality standards.
Inpatient treatment program.
Residential treatment.
Partial hospitalization program.
Detox.
Outpatient treatment.
Medication management counseling.
Support group therapy.
Does TriWest Cover Medications?
TriWest covers medications that may help ease withdrawal symptoms. One such program that involves medications is Medication-Assisted Treatment (MAT). MAT programs use both medication and behavioral therapy to help with (usually) an opioid use disorder.
The FDA approved three drugs for MAT purposes. These drugs are as follows:
Buprenorphine: used to treat opioid addiction.
Naltrexone: used for opioid or alcohol use disorder.
Regional Networks
CCN is comprised of five regional networks that serve as the contract vehicle for VA to purchase care for Veterans from community providers. The existing Patient-Centered Community Care (PC3) network will transition over time to allow for CCN implementation to occur region-by-region in a phased approach.